Several scoring systems are used in neurosurgical patients to assess various aspects of their condition, predict outcomes, and guide treatment decisions. Here are some commonly used scoring systems in neurosurgery:
1. Glasgow Coma Scale (GCS):
The GCS assesses a patient’s level of consciousness based on eye, verbal, and motor responses. It is widely used to evaluate the severity of traumatic brain injury and other neurological conditions.

The Glasgow Coma Scale (GCS) is a neurological assessment tool that assigns a score based on a patient’s eye, verbal, and motor responses. The total GCS score, ranging from 3 to 15, helps quantify the level of consciousness and neurological impairment. A higher score indicates a higher level of consciousness and responsiveness, while a lower score suggests more severe impairment.
2. Hunt and Hess Grading Scale:
This scale is used to assess the severity of subarachnoid hemorrhage due to an aneurysm. It helps predict outcomes and guide treatment decisions, including the need for surgical intervention.
It is a clinical classification system used to assess the severity of subarachnoid hemorrhage (SAH) due to a ruptured cerebral aneurysm. It helps in predicting patient overcomes and guiding treatment decisions. The scale ranges from Grade 0 (no symptoms) to Grade V (deep coma or brain death). Here’s a table summarizing the Hunt and Hess Grading Scale:
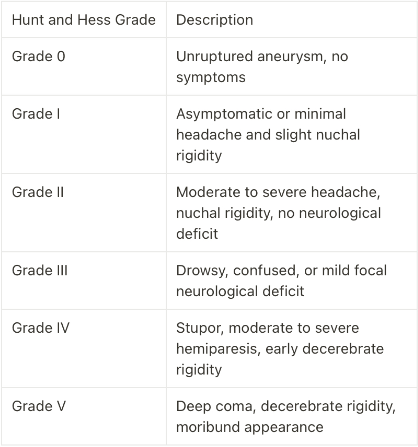
Each grade represents a different level of neurological impairment and helps clinicians classify the severity of SAH. The higher the grade, the more severe the condition, and the worse the prognosis tends to be. Neurosurgeons and medical teams use this scale to guide treatment decisions and predict patient outcomes after SAH.
3. Fisher Scale:
The Fisher Scale is used to classify the severity of subarachnoid hemorrhage based on the amount of blood detected on a CT scan. It helps determine the risk of complications and mortality.

Discussion:
The Fisher Scale is used to classify the amount of blood seen on a non-contrast CT scan following subarachnoid hemorrhage (SAH). It helps predict the risk of vasospasm and overall outcomes, while higher grades suggest a higher risk of vasospasm and poorer outcomes.
4. Modified Rankin Scale (mRS):
The mRS assesses a patient’s functional disability after a stroke or other neurological event. It ranges from 0 (no symptoms) to 6 (dead), helping in outcome assessment and treatment planning.

Discussion:
The Modified Rankin Scale (mRS) assesses disability or dependence in daily activities for people who have experienced a stroke or other neurological disorders. It is commonly used in stroke research and clinical practice to communicate the functional outcomes of patients. Lower scores indicate better functional status and independence, while higher scores represent greater disability and dependence.
5. National Institutes of Health Stroke Scale (NIHSS):
This scale is used to assess the severity of a stroke’s neurological deficits. It quantifies various aspects of neurological function, aiding in diagnosis and treatment decisions.
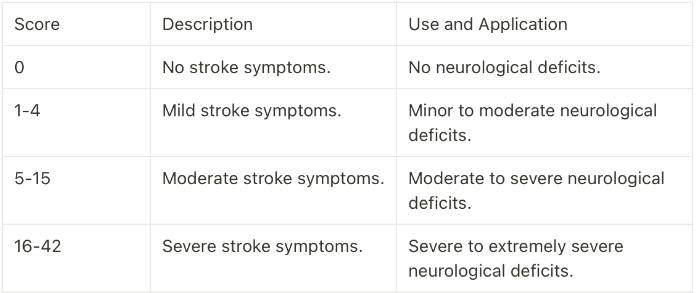
Discussion:
The National Institutes of Health Stroke Scale (NIHSS) quantifies the severity of a stroke and measures neurological deficits. It is used to determine treatment decisions and assess the effectiveness of interventions in acute stroke care. Lower scores indicate milder symptoms and fewer deficits, while higher scores suggest more severe symptoms and deficits.
6. Hammersmith Functional Motor Scale (HFMS):
The HFMS is used to assess motor function in patients with neuromuscular disorders such as spinal muscular atrophy. It helps monitor disease progression and response to treatment.
7. Pediatric Glasgow Coma Scale (PGCS):
Similar to the adult GCS, the PGCS is used to assess the level of consciousness in pediatric patients. It considers age-appropriate verbal and motor responses.
8. Modified Barthel Index (MBI):
The MBI assesses a patient’s ability to perform activities of daily living, which is crucial in evaluating functional outcomes after neurosurgery or stroke.
9. Intracerebral Hemorrhage (ICH) Score:
This score helps predict the risk of mortality and functional outcomes in patients with intracerebral hemorrhage. It considers factors like age, GCS score, hematoma volume, and intraventricular hemorrhage.
10. Aneurysm Clipping Grading Scales (e.g., ISUIA, ISAT):
These scales are used to assess the suitability of aneurysm treatment (clipping or coiling) based on factors like aneurysm size, location, and patient characteristics.
11. Spinal Cord Injury (SCI) Scoring Systems (e.g., ASIA Impairment Scale):
Scoring systems like the ASIA Impairment Scale assess the severity of spinal cord injuries, helping determine the extent of motor and sensory deficits.
12. Pittsburgh Sleep Quality Index (PSQI):
The PSQI assesses sleep quality and disturbances, which are relevant in various neurological conditions and can impact recovery and quality of life.
These scoring systems play crucial roles in the assessment, management, and prognosis of neurosurgical patients. The choice of the specific scale depends on the patient’s condition and the clinical context.

