Neurosurgical procedures, particularly those involving the dura mater, present unique challenges for anesthesiologists due to the intricate relationship between intracranial pressure (ICP), venous air embolism (VAE), and sympathetic nervous system activation. Managing hemodynamic disturbances during these critical phases is essential to optimize patient outcomes and prevent severe complications.
1. Understanding Intracranial Pressure (ICP) Dynamics
1.1 Hemodynamics During Dural Opening
The opening of the dura mater in neurosurgery results in a rapid release of cerebrospinal fluid (CSF), which typically leads to a significant decrease in ICP. This sudden reduction can transiently increase cerebral perfusion pressure (CPP) by widening the gap between mean arterial pressure (MAP) and ICP. However, this decrease in ICP may cause brain tissue to bulge, especially in patients with pre-existing cerebral edema. This phenomenon can trigger the “Cushing reflex,” characterized by systemic hypotension and bradycardia due to an exaggerated sympathetic response.
1.2 Hemodynamics During Dural Closure
As the dura is closed, the risk of ICP elevation resurfaces, particularly if residual edema or ongoing CSF accumulation exists. An increase in ICP during this phase can compromise CPP, potentially leading to Cushing’s triad—a critical combination of hypertension, bradycardia, and irregular respirations, indicating significant intracranial hypertension. Anesthesiologists must be vigilant during this stage, as failure to manage rising ICP effectively could result in life-threatening complications such as cerebral herniation or ischemic injury.
2. Venous Air Embolism (VAE) Risks and Management
2.1 Elevated Risk During Dural Opening
VAE is a significant risk during the dural opening, particularly in patients positioned in the sitting or semi-sitting posture. The negative pressure created within venous structures during this phase can allow air to enter the venous system, leading to a range of complications depending on the volume of air introduced. Symptoms of VAE can vary from transient hypoxemia to severe cardiovascular collapse, necessitating immediate recognition and intervention by the anesthesiology team.
2.2 Pathophysiology of VAE
Once air enters the pulmonary circulation, it can lead to increased pulmonary artery pressure and reduced cardiac output, placing significant strain on the right ventricle. The presence of a patent foramen ovale (PFO) further complicates the situation, as air may enter the systemic circulation, leading to catastrophic outcomes such as stroke or myocardial infarction. Prompt detection and management strategies, including precordial Doppler monitoring and positive end-expiratory pressure (PEEP), are critical to mitigating the effects of VAE.
3. Hemorrhagic Complications During Dural Closure
3.1 Mechanisms and Risk Factors
The process of dural closure poses a risk of hemorrhagic complications, particularly if fragile blood vessels are inadvertently trapped during suturing. Inadequate hemostasis in such cases can lead to significant blood loss and subsequent hemodynamic instability. Anesthesiologists must be prepared to manage these complications, which are more likely in patients with delicate tissue structures .
4. Sympathetic Nervous System Activation
4.1 Response to Dural Manipulation
The dura mater is densely innervated, and its manipulation can activate the sympathetic nervous system, leading to acute hypertensive episodes and increased heart rates. These stress responses are particularly concerning in patients with pre-existing cardiovascular conditions, making it crucial for anesthesiologists to closely monitor and manage these sympathetic outbursts to ensure patient safety.
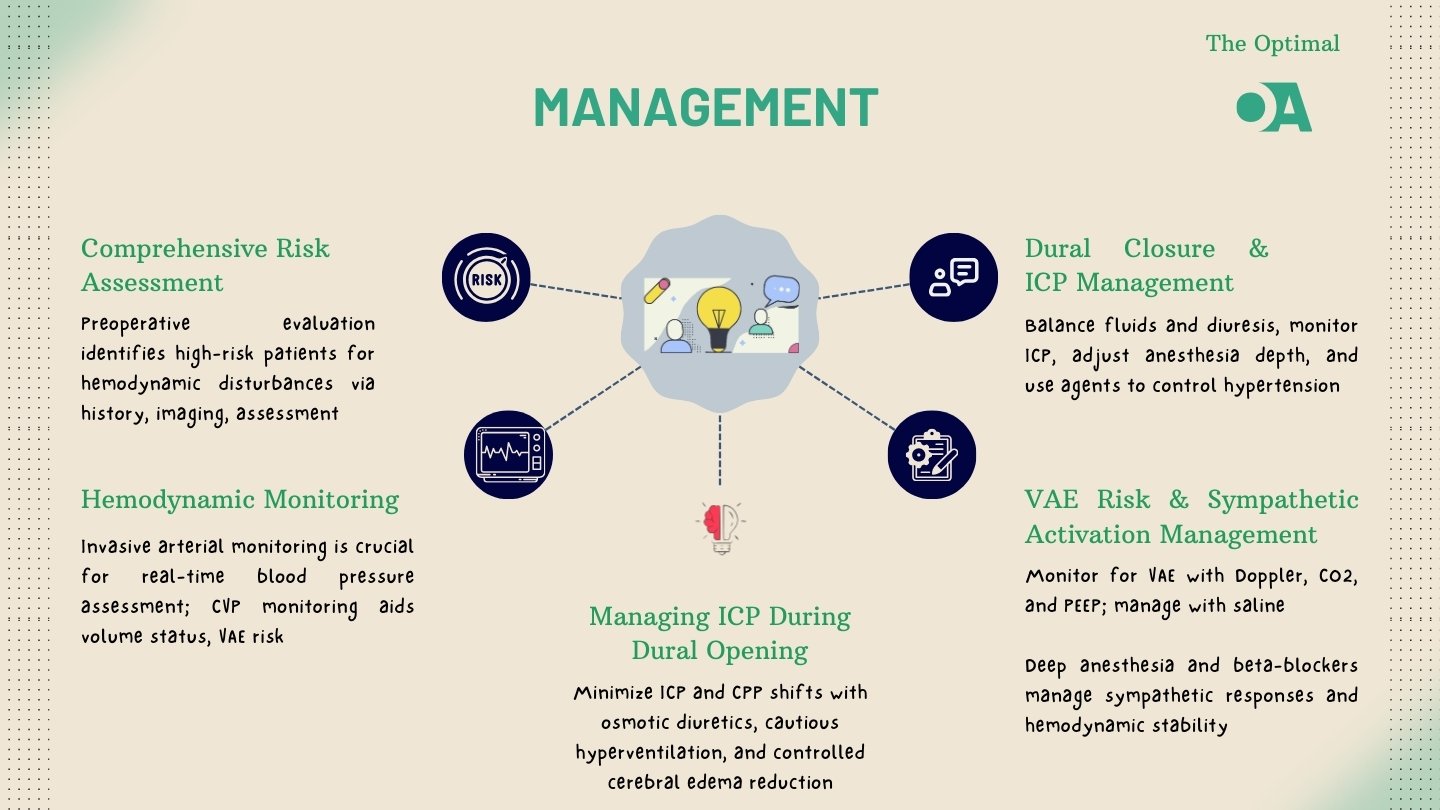
5. Anesthetic Management Strategies
5.1 Preoperative Assessment and Preparation
Effective management of hemodynamic disturbances begins with a thorough preoperative assessment. Identifying patients at risk for elevated ICP or significant cerebral edema is essential. The use of invasive monitoring, such as arterial pressure and central venous pressure monitoring, provides real-time data that can guide anesthetic management during the procedure.
5.2 Intraoperative Anesthetic Management
To mitigate ICP fluctuations, the administration of osmotic diuretics like mannitol before dural opening is recommended. Additionally, hyperventilation may be cautiously employed to reduce cerebral blood flow and, consequently, ICP. To minimize the risk of VAE, maintaining a positive end-expiratory pressure (PEEP) and using precordial Doppler monitoring can be effective. In the event of an embolic event, immediate measures such as filling the surgical field with saline and aspirating air from the right atrium should be initiated.
During dural closure, careful management of fluid balance is crucial to prevent excessive increases in ICP. Continuous ICP monitoring can help inform anesthetic depth adjustments, with agents like remifentanil being particularly useful for controlling hypertensive events.
5.3 Postoperative Care and Monitoring
Postoperatively, close monitoring of ICP and hemodynamic stability is essential. Effective pain management, regular neuroimaging, and vigilant assessment for potential complications can significantly improve recovery outcomes. Ensuring a smooth transition from intraoperative to postoperative care is vital for optimizing patient outcomes .
Conclusion
Managing hemodynamic disturbances during the opening and closure of the dura mater in neurosurgical procedures is a complex and critical task for anesthesiologists. By understanding the pathophysiological mechanisms involved and implementing targeted anesthetic strategies, anesthesiologists can significantly enhance patient safety and procedural success. Continuous education, adherence to updated guidelines, and a collaborative approach are key to achieving optimal outcomes in these challenging surgical environments.
References:
- Intracranial Pressure Monitoring – StatPearls – NCBI Bookshelf, https://www.ncbi.nlm.nih.gov/books/NBK542298/
- Venous air embolism: a review., https://www.semanticscholar.org/paper/97269a97cae84febba0322c7d803711a2d673046
- Venous Air Embolism: Background, Pathophysiology, Etiology, https://emedicine.medscape.com/article/761367-overview
- Symptomatic Intracranial Hemorrhage after Dural Tear in Spinal …, https://pubmed.ncbi.nlm.nih.gov/33640532/
- Intracranial hemorrhage following lumbar spine surgery – PMC – NCBI, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3463703/
- Dural sealants for the management of cerebrospinal fluid leakage …, https://www.tandfonline.com/doi/full/10.1080/17434440.2019.1626232
- THE EXPLORATION OF POTENTIAL SPINAL MANIPULATION …, https://journal.parker.edu/article/94424-the-exploration-of-potential-spinal-manipulation-effects
- Effect of preoperative fluid therapy on hemodynamic stability during …, https://pubmed.ncbi.nlm.nih.gov/31240711/
- Perioperative Patients With Hemodynamic Instability – NCBI, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10916753/
- ACC/AHA Guideline Update for Perioperative Cardiovascular …, https://www.ahajournals.org/doi/10.1161/circ.105.10.1257
- Preoperative Evaluation and Risk Management – PMC – NCBI, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2780235/
- Perioperative Patients With Hemodynamic Instability, https://journals.lww.com/anesthesia-analgesia/fulltext/2024/04000/perioperative_patients_with_hemodynamic.4.aspx
- Hemodynamic management during anesthesia in adults – UpToDate, https://www.uptodate.com/contents/hemodynamic-management-during-anesthesia-in-adults
- Hemodynamic management during anesthesia in adults – MediLib, https://medilib.ir/uptodate/show/94532
- Anesthesia for craniotomy in adults – UpToDate, https://www.uptodate.com/contents/anesthesia-for-craniotomy-in-adults
- The relationships between anesthesia, hemodynamics and outcome, https://www.cambridge.org/core/books/perioperative-hemodynamic-monitoring-and-goal-directed-therapy/relationships-between-anesthesia-hemodynamics-and-outcome/E013D60714A976C872D32261CFD7DFA4