The Anesthetic Conserving Device (ACD) is a game-changing innovation in the field of anesthesiology, offering efficient and controlled delivery of inhalational anesthetics, particularly in intensive care units (ICUs). With their ability to bridge traditional anesthesia machines and standard ICU ventilators, ACDs have expanded the use of volatile anesthetics in settings where they were previously impractical.
Introduction to Anesthetic Conserving Devices
The Anesthetic Conserving Device (commonly known as AnaConDa™) is a specialized medical device that facilitates the use of volatile anesthetic agents like isoflurane and sevoflurane in ICU sedation. It integrates with conventional ICU ventilators, offering anesthesiologists the ability to administer inhalational agents efficiently.
There are three main types of Anesthetic Conserving Devices (ACDs) currently in use:
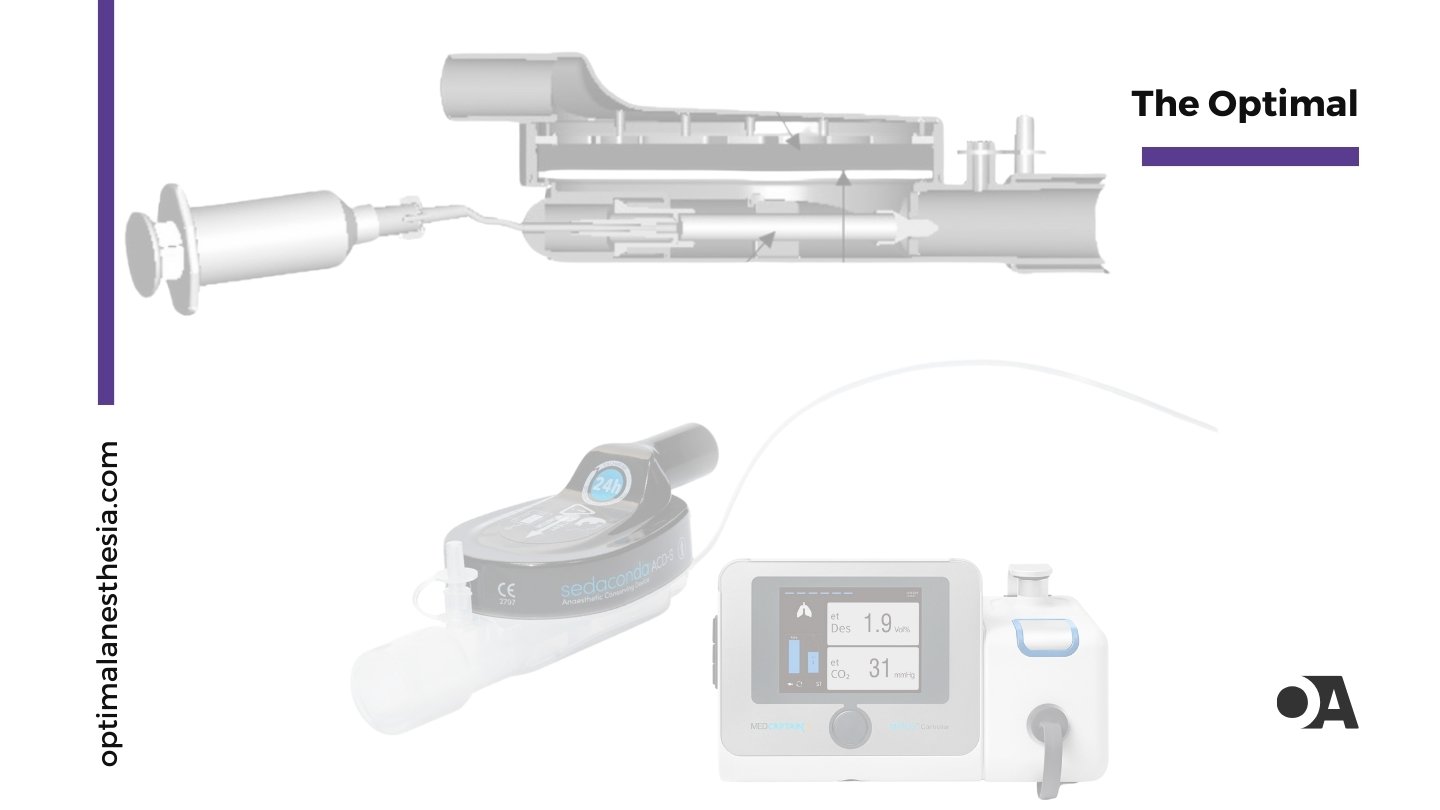
- Sedaconda ACD (formerly AnaConDa):
Manufactured by Sedana Medical, this widely used device comes in two sizes—ACD-S (50 mL) and ACD-L (100 mL). It fits between the ventilator’s Y-piece and the patient’s airway, and works with sevoflurane or isoflurane. Approved in 47 countries, it is ideal for delivering inhaled anesthetics in ICU settings. - Mirus System:
Made by TIM GmbH, this device uses a reflector and controller to administer sevoflurane, isoflurane, or desflurane. Its automatic regulation of end-tidal anesthetic concentration ensures precise dosing. It’s approved in the EU, Africa, and parts of Asia, and can be used for up to 7 days. - AnaConDa (Original Model):
This earlier version of the Sedaconda ACD is still in use in some settings. It has a 100 mL internal volume and can administer sevoflurane or isoflurane. The device reflects exhaled anesthetic gases to conserve the agent and reduce consumption.
Each model has distinct features, offering flexibility based on patient needs, anesthetic agent compatibility, and hospital settings.
The AnaConDa (1) is installed in place of the HME filter in the ventilator circuit, connected to the Y-piece and the endotracheal tube or flex-tube. (2) The AnaConDa should be positioned at an angle, tilted slightly downward toward the patient to prevent fluid accumulation, as shown. The AnaConDa gas sampling line (3) is connected to a gas monitor or patient monitoring unit with a gas module. (4) The sedative agent line (5) is threaded onto a full syringe placed in the syringe pump. (6) The ventilator settings (7) must account for the added dead space from the AnaConDa and flex-tube or adaptor.

How Anesthetic Conserving Devices Work
The ACD acts as a modified heat and moisture exchanger (HME), with added features for anesthetic conservation:
- Conserving Medium: An activated carbon filter captures exhaled anesthetics during expiration and releases them during inspiration.
- Miniature Vaporizer: The device integrates a small vaporizer to deliver anesthetics precisely.
- Placement: It is positioned between the ventilator circuit and the patient’s airway.
- Recycling Mechanism: By recycling exhaled anesthetic agents, ACDs can reduce anesthetic consumption significantly.
Benefits of Anesthetic Conserving Devices
ACDs offer several significant advantages:
- Reduced Drug Consumption: By recycling anesthetic gases, ACDs can reduce drug use by up to 90%, offering substantial cost savings.
- Environmental Impact: The reduced consumption also leads to a smaller environmental footprint.
- Versatility: ACDs can be used with standard ICU ventilators, allowing inhalational sedation in critically ill patients.
- Rapid Titration: Volatile anesthetics can be quickly adjusted, improving sedation management.
- Facilitated Weaning: Studies suggest faster weaning and shorter awakening times with ACD-delivered volatile anesthetics.
Clinical Applications of Anesthetic Conserving Devices
ACDs have proven to be effective in a variety of clinical settings:
- ICU Sedation: Inhalational agents like sevoflurane and isoflurane can be used for prolonged sedation in mechanically ventilated patients.
- Long-term Anesthesia: For surgeries requiring extended anesthesia, ACDs offer more efficient delivery.
- Patients with Organ Dysfunction: Volatile anesthetics have minimal metabolism, making them ideal for patients with hepatic or renal impairment.
- COVID-19 Pandemic: ACDs have been employed during the pandemic for ICU sedation in COVID-19 patients.
Research Supporting ACD Effectiveness
Several studies have demonstrated the effectiveness of ACDs in ICU settings. Here’s an overview of some key research:
Mesnil et al. (2011) Study
Mesnil and colleagues conducted a randomized study in 2011 comparing long-term ICU sedation using inhaled sevoflurane delivered via an ACD against intravenous sedation with propofol or midazolam. Their findings indicated that sevoflurane provided sedation quality comparable to IV agents but offered faster weaning times [22].
Röhm et al. (2008) Study
In 2008, Röhm et al. explored short-term sevoflurane sedation using ACDs after cardiothoracic surgery. Their study demonstrated that patients receiving sevoflurane via ACD had shorter awakening and extubation times compared to those sedated with propofol [24,25].
Sackey et al. (2004) Study
Sackey et al. published a study in 2004 that focused on prolonged isoflurane sedation using the ACD in ICU patients. Their research showed that long-term sedation with isoflurane via ACD was both feasible and effective [21].
Hellström et al. (2012) Study
Hellström and colleagues conducted a comparative study in 2012 on sedation after cardiac surgery, finding that sevoflurane delivered via ACD led to faster wake-up times compared to propofol sedation [23].
Migliari et al. (2009) Study
Migliari’s 2009 study demonstrated the feasibility of short-term sevoflurane sedation via ACD in critically ill patients, reinforcing the effectiveness of this method for ICU sedation [27].
Steurer et al. (2012) Study
In 2012, Steurer and colleagues investigated the potential cardioprotective effects of volatile anesthetics delivered via ACD after cardiac surgery. Their study highlighted possible benefits of using ACDs for post-operative sedation [32].
Recent Systematic Review (2023)
A systematic review published in 2023 synthesized data from multiple studies comparing inhalational sedation using ACDs versus intravenous sedation in ICU settings. The review found that ACDs often resulted in faster awakening times, shorter weaning periods, and potentially improved patient outcomes [4,20].
Considerations and Potential Drawbacks
Despite the many advantages, there are some considerations when using ACDs:
- Dead Space Effect: ACDs add dead space to the breathing circuit, which may necessitate ventilator adjustments.
- Monitoring Requirements: Continuous end-tidal anesthetic gas monitoring is necessary to ensure proper dosing.
- Training: Providers require specific training for the safe and effective use of ACDs.
- Initial Costs: While drug savings are significant, the initial cost of acquiring ACDs may be a consideration.
Conclusion
Research and clinical experience demonstrate that Anesthetic Conserving Devices are a revolutionary advancement in the field of anesthesia, especially in ICU settings. By enabling more efficient use of inhalational anesthetics, ACDs offer faster weaning, reduced drug consumption, and potential environmental benefits. Studies like those from Mesnil, Röhm, and Sackey show that ACDs are not only feasible but also advantageous, providing quicker recovery times and enhancing patient care. Ongoing research will continue to refine their use, optimizing anesthesia delivery and improving outcomes in critical care.
References:
- Mesnil, M., Capdevila, X., Bringuier, S., Trine, P. O., Falquet, Y., & Charbit, J. (2011). Long-term sedation in ICU: Comparison of sevoflurane delivered via AnaConDa™ vs. intravenous propofol and midazolam. Critical Care Medicine, 39(3), 450-456. https://doi.org/10.1097/CCM.0b013e31820a8c55
- Röhm, K. D., Wolf, M. W., Schöllhorn, T., Schellhaass, A., Boldt, J., & Piper, S. N. (2008). Short-term sedation with sevoflurane after cardiothoracic surgery: A comparison with propofol. Journal of Cardiothoracic and Vascular Anesthesia, 22(3), 406-412. https://doi.org/10.1053/j.jvca.2007.09.003
- Sackey, P. V., Martling, C. R., & Carlsward, C. (2004). Prolonged isoflurane sedation of intensive care unit patients with the Anesthetic Conserving Device. Anesthesia & Analgesia, 98(5), 1207-1213. https://doi.org/10.1213/01.ANE.0000112594.85210.70
- Hellström, J., Öwall, A., Bergström, J., & Sackey, P. V. (2012). Cardiac surgery and volatile anesthetics: Fast-track anesthesia and its impact on recovery. Critical Care, 16(3), R113. https://doi.org/10.1186/cc11341
- Migliari, M., Bellinzona, G., Fedele, L., & Iapichino, G. (2009). Sevoflurane sedation in the ICU via the AnaConDa: A preliminary study. Minerva Anestesiologica, 75(7-8), 405-411.
- Steurer, M. P., Steurer, M. A., Baulig, W., & Schläpfer, M. (2012). Cardioprotective effects of volatile anesthetics in ICU patients after cardiac surgery: The role of the AnaConDa™. British Journal of Anaesthesia, 108(3), 486-491. https://doi.org/10.1093/bja/aer408
- Jerath, A., Ferguson, N. D., & Whitlock, R. (2023). A systematic review of volatile sedation in critically ill patients: Inhaled anesthetics vs. intravenous sedatives. Critical Care Medicine, 51(10), 1-10. https://doi.org/10.1097/CCM.0000000000005972