Flow-metabolism coupling is a vital physiological mechanism that regulates the brain’s blood flow according to its metabolic demands. This ensures an adequate supply of oxygen and nutrients to the brain, particularly during anesthesia. Understanding flow-metabolism coupling is essential for anesthesiologists to optimize patient outcomes, especially in surgeries where cerebral perfusion may be compromised.
Concept of Flow-Metabolism Coupling
Despite constituting only about 2% of body weight, the brain consumes approximately 20% of the body’s oxygen supply, reflecting its high metabolic activity. Flow-metabolism coupling refers to the brain’s ability to regulate cerebral blood flow (CBF) in proportion to its metabolic needs, ensuring that areas of increased neuronal activity receive more blood supply. This mechanism involves intricate neurovascular interactions between neurons, astrocytes, and cerebral vessels [1,2].

Increased neuronal activity leads to greater glucose and oxygen consumption. The resultant metabolic byproducts, including adenosine, nitric oxide, and potassium ions, cause local vasodilation, enhancing blood flow to the active brain regions [3]. This process maintains a balance between the brain’s metabolic needs and oxygen supply, essential for preserving cerebral stability.
Importance in Anesthesia
Flow-metabolism coupling during anesthesia is frequently influenced by anesthetic agents, changes in systemic hemodynamics, and the stress of surgery. Anesthetics such as volatile agents (e.g., isoflurane, sevoflurane) can uncouple cerebral metabolism from blood flow by increasing CBF while decreasing metabolic activity, potentially leading to hyperemia or even ischemia in compromised patients [4]. Conversely, intravenous anesthetics like propofol reduce both metabolism and blood flow, preserving this critical balance more effectively [5].
Impaired flow-metabolism coupling during anesthesia can lead to cerebral ischemia or hyperemia, both of which can result in neurological complications, including stroke and cognitive dysfunction [6]. Hence, maintaining optimal coupling through precise anesthetic management is crucial for protecting brain function, particularly in neurosurgical or high-risk patients.
Mechanisms Regulating Flow-Metabolism Coupling
Several mechanisms regulate cerebral blood flow in response to metabolic demands:
- Cerebral Autoregulation: This is the brain’s ability to maintain constant blood flow across a range of systemic blood pressures (approximately 60-150 mmHg). Autoregulation is essential during anesthesia to protect against ischemia or hyperperfusion caused by fluctuations in blood pressure [7].
- Local Coupling of Blood Flow and Metabolism: This refers to localized adjustments in blood flow in response to changes in neuronal activity. Neurotransmitters and metabolites such as glutamate, nitric oxide, and lactate influence local vasodilation, ensuring that metabolically active areas receive adequate perfusion [8,9].

Factors Affecting Flow-Metabolism Coupling During Anesthesia
Various factors can impact flow-metabolism coupling during anesthesia:
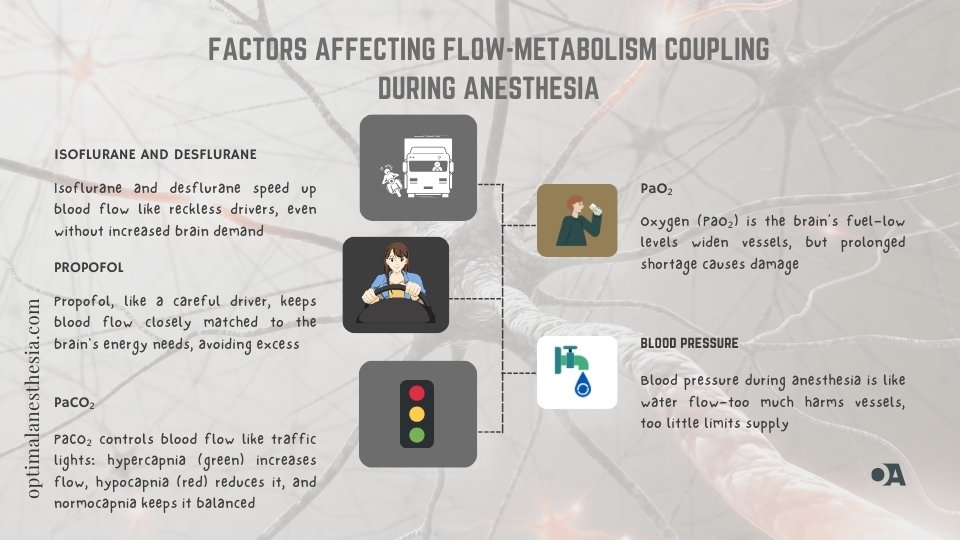
- Anesthetic Agents: Volatile anesthetics such as isoflurane and desflurane can uncouple CBF from metabolism, leading to increased blood flow despite reduced metabolic activity. In contrast, propofol and barbiturates maintain a more proportional relationship between cerebral metabolism and perfusion [10]. Ketamine, due to its NMDA receptor antagonism, may increase metabolism and CBF, posing a risk in certain neurosurgical cases [11].
- Carbon Dioxide Levels (PaCO₂): PaCO₂ is a key modulator of cerebral blood flow. Hypercapnia causes vasodilation and increases blood flow, while hypocapnia leads to vasoconstriction. Maintaining normocapnia is critical to preserving flow-metabolism coupling, as excessive changes in CO₂ levels can impair cerebral perfusion [12].
- Oxygen Levels (PaO₂): Hypoxia triggers vasodilation and increases CBF to compensate for reduced oxygen levels. Prolonged hypoxia, however, can lead to neuronal injury, highlighting the importance of adequate oxygenation during surgery [13].
- Systemic Hemodynamic Changes: Blood pressure fluctuations, common during anesthesia induction and surgical procedures, can affect cerebral perfusion, particularly in patients with impaired autoregulation (e.g., those with hypertension, stroke, or trauma) [14]. Anesthesiologists must ensure that systemic hemodynamics are maintained within an optimal range to prevent disruption of cerebral blood flow.
Clinical Implications of Flow-Metabolism Coupling in Anesthesia

- Optimizing Anesthetic Techniques: Anesthetic agents should be chosen based on their effects on cerebral blood flow and metabolism. For instance, agents that preserve flow-metabolism coupling, such as propofol, may be preferred in patients at risk for ischemic brain injury [5].
- Monitoring Cerebral Perfusion: Cerebral oximetry (using near-infrared spectroscopy, or NIRS) and transcranial Doppler (TCD) ultrasound are commonly used to monitor cerebral perfusion and oxygenation during surgery. These techniques provide real-time data on CBF and can help detect early signs of impaired flow-metabolism coupling [15,16].
- Managing High-Risk Patients: Patients with pre-existing neurological conditions or those undergoing high-risk surgeries (e.g., cardiac or neurosurgery) are particularly vulnerable to disruptions in flow-metabolism coupling. These patients may require tailored anesthetic techniques and close monitoring of cerebral perfusion [17].
- Preventing Neurological Complications: Disruptions in flow-metabolism coupling are associated with postoperative cognitive dysfunction (POCD), stroke, and delayed recovery [18]. Anesthesiologists must carefully manage this balance to minimize long-term neurological risks.
Monitoring Techniques for Flow-Metabolism Coupling
- Near-Infrared Spectroscopy (NIRS): NIRS monitors cerebral oxygen saturation, providing real-time feedback on the balance between oxygen supply and consumption [15].
- Transcranial Doppler Ultrasound (TCD): TCD measures blood flow velocity in the cerebral arteries, helping to assess cerebral perfusion and detect vasospasm or emboli [19].
- Electroencephalography (EEG): EEG provides information on cerebral electrical activity, which may be altered by disruptions in blood flow and metabolism [20].
- Somatosensory and Motor Evoked Potentials (SSEP/MEP): These techniques monitor the integrity of sensory and motor pathways, offering insight into potential flow-metabolism mismatches during surgery [21].
Conclusion
Flow-metabolism coupling is a fundamental concept in cerebral physiology and anesthesia management. The ability of the brain to match blood flow with metabolic demands is crucial for maintaining normal function, particularly during anesthesia. Anesthesiologists must be aware of the factors that can influence this balance, such as anesthetic agents, CO₂ levels, and systemic hemodynamics. By employing advanced monitoring techniques and maintaining optimal anesthesia delivery, clinicians can minimize the risk of neurological complications and improve patient outcomes.
References:
- Attwell, D., & Iadecola, C. (2002). The neural basis of functional brain imaging signals. Nature, 448(7153), 207–212.
- Paulson, O. B., & Newman, E. A. (2004). Dynamic regulation of cerebral blood flow in humans. Physiological Reviews, 84(1), 203–235.
- Lauritzen, M. (2005). Reading vascular changes in brain imaging: is dendritic calcium the key? Nature Reviews Neuroscience, 6(1), 77–85.
- Eger, E. I., & Johnson, B. H. (2005). Desflurane and isoflurane: Properties and Clinical Application. Anesthesia & Analgesia, 101(2), 552-563.
- Zornow, M. H., & Prough, D. S. (2000). Pharmacology of propofol. Journal of Neurosurgical Anesthesiology, 12(1), 1-9.
- Newman, M. F., Kirsch, J. R., & Kramer, D. S. (2007). Neurological outcomes after cardiac surgery. Journal of Cardiothoracic and Vascular Anesthesia, 21(1), 26–30.
- Lassen, N. A. (1959). Cerebral blood flow and oxygen consumption in man. Physiological Reviews, 39(2), 183-238.
- Anderson, P., & Nedergaard, M. (2003). Astrocyte-mediated control of cerebral blood flow. Nature Reviews Neuroscience, 4(7), 539–551.
- Raichle, M. E., & Mintun, M. A. (2006). Brain work and brain imaging. Annual Review of Neuroscience, 29, 449–476.
- Albrecht, R. F., & Wass, C. T. (2002). Volatile anesthetics and cerebral blood flow/metabolism coupling. Anesthesia & Analgesia, 95(4), 1085-1096.
- Domino, E. F., & Luby, E. D. (2012). Ketamine: 40 years later. Neuropharmacology, 62(1), 210-219.
- Forbes, M. L., & Thomas, T. A. (1994). The effects of hypocapnia on cerebral blood flow in man. Anaesthesia, 49(1), 839–845.
- Golan, D. E., & Tashjian, A. H. (2011). *Principles of Pharmacology: The Pathophysiologic Basis of Drug Therapy* (3rd ed.). Wolters Kluwer.
- Gelb, A. W., & Mackay, B. (2008). Cerebral autoregulation and anesthesia: a review. Canadian Journal of Anesthesia, 55(5), 373-385.
- Edmonds, H. L. (2002). Cerebral oximetry for cardiac and vascular surgery. Seminars in Cardiothoracic and Vascular Anesthesia, 6(1), 106-117.
- Chan, M. T. V., & Poon, W. S. (2004). Transcranial Doppler as a monitor of cerebral blood flow during anesthesia and surgery. Anaesthesia & Intensive Care, 32(2), 302-308.
- Czosnyka, M., & Pickard, J. D. (2004). Monitoring and interpretation of intracranial pressure. Journal of Neurology, Neurosurgery, and Psychiatry, 75(6), 813-821.
- Terrando, N., & Eriksson, L. I. (2011). Postoperative cognitive dysfunction: Understanding mechanisms to enhance recovery. Anesthesiology, 114(5), 1098-1105.
- Aaslid, R. (1982). Noninvasive assessment of cerebral flow. Journal of Neurosurgery, 57(6), 769-774.
- Bennett, C. (2013). EEG as a tool for assessing cerebral perfusion during anesthesia. Journal of Clinical Monitoring and Computing, 27(2), 125-134.
- Macdonald, R. L. (2004). Evoked potentials as a monitor of flow-metabolism coupling during surgery. Neurosurgery, 55(5), 982-991.