Patients undergoing neurosurgical procedures may be placed in various positions depending on the nature of the surgery, the specific area of the brain or spine being operated on, and the surgical approach chosen by the neurosurgeon. Common patient positions for neurosurgery include:
1. Supine Position (Flat on the Back):
– Used for a wide range of neurosurgical procedures, including craniotomies (skull surgeries) and some spinal surgeries.
– Provides easy access to the patient’s head for intracranial surgeries.
– The patient’s head may be secured in a headrest or held in place with pins or clamps for stability.
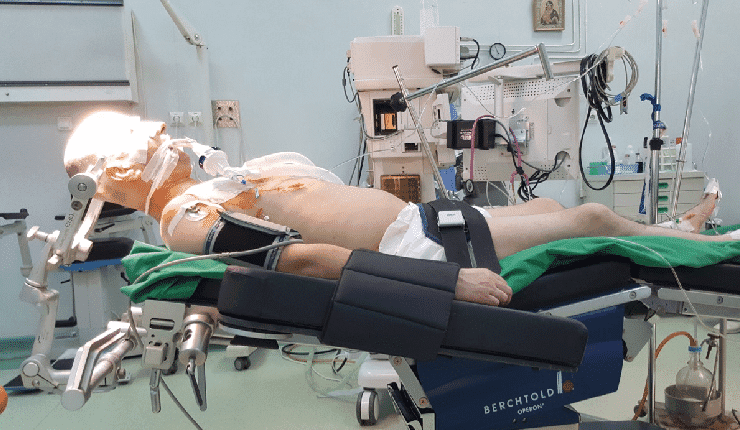
2. Prone Position (Face Down):
– Frequently used for spinal surgeries, particularly those involving the cervical (neck) or thoracic (upper back) spine.
– Allows access to the posterior (back) aspect of the spine for decompression, fusion, or instrumentation procedures.
– Special padding and positioning devices are used to protect and support the patient’s head and body.
3. Lateral Position (Sideways):
– Used for surgeries involving the lateral aspects of the brain or spine.
– For brain surgeries, it provides access to lesions or structures located on the sides of the brain.
– In spinal surgeries, it may be used for approaches to the lateral or anterolateral spine.
4. Sitting Position:
– Occasionally employed for posterior fossa brain surgeries, such as for the removal of tumors located at the base of the skull.
– Requires special head fixation and careful monitoring of blood pressure to prevent cerebrospinal fluid (CSF) leakage and ensure cerebral perfusion.
5. Semi-Sitting Position:
– Similar to the sitting position but with the patient at a less steep angle.
– May be used for some posterior fossa surgeries or when sitting position is contraindicated.
6. Trendelenburg Position (Head Down):
– Utilized to facilitate venous drainage during some intracranial procedures.
– Tilting the operating table so that the patient’s head is lower than their feet can help reduce intracranial pressure.
7. Reverse Trendelenburg Position (Head Up):
– Occasionally used for intracranial surgeries when the surgeon needs to access the upper parts of the brain.
– May also be employed for some spinal surgeries for better visualization.
8. Park-Bench Position:
– Specific to certain spinal surgeries, such as scoliosis correction.
– The patient’s body is contoured to mimic a park bench, allowing for spinal instrumentation and fusion.
It’s important to note that patient positioning in neurosurgery requires meticulous care to avoid complications related to pressure sores, nerve injuries, or circulatory issues. The choice of position depends on the surgical goals and patient factors, and the anesthesia and surgical teams work closely to ensure patient safety and optimal surgical access.
Here’s a discussion of common problems associated with various patient positions in neurosurgical procedures and preventive measures to mitigate these issues:
1. Supine Position:
– Problems: Risk of pressure sores, potential difficulties in achieving optimal surgical access in some cases.
– Prevention: Frequent monitoring and padding to prevent pressure ulcers. Proper head fixation for stability and positioning devices as needed.
2. Prone Position:
– Problems: Risk of facial edema, eye injuries, brachial plexus injury, and pressure ulcers on bony prominences.
– Prevention: Protective measures for eyes and face, careful padding, use of positioning devices, and frequent repositioning to relieve pressure points.
3. Lateral Position:
– Problems: Risk of brachial plexus injury, pressure ulcers, and difficulties in maintaining anesthesia and ventilation.
– Prevention: Proper padding, use of pressure-relief mattresses, and vigilant monitoring of limb positioning. Coordination between anesthesia and surgical teams for airway management.
4. Sitting Position:
– Problems: Risk of air embolism, venous congestion, and complications associated with cerebrospinal fluid (CSF) leakage.
– Prevention: Careful head fixation and meticulous attention to airway management. Monitoring of intracranial pressure and vigilance in preventing CSF leakage.
5. Semi-Sitting Position:
– Problems: Similar to the sitting position, but with a reduced risk of complications.
– Prevention: As in the sitting position, proper head fixation and monitoring are essential, with extra precautions for airway management and CSF leakage prevention.
6. Trendelenburg Position:
– Problems: Risk of facial edema, increased intracranial pressure, and potential complications in patients with cardiovascular issues.
– Prevention: Monitoring of intracranial pressure, careful fluid management, and frequent checks for facial edema. Vigilance in maintaining cardiovascular stability.
7. Reverse Trendelenburg Position:
– Problems: Potential difficulties in achieving optimal surgical access, patient discomfort.
– Prevention: Adequate padding and monitoring of patient comfort. Coordination with the surgical team to ensure adequate visualization.
8. Park-Bench Position:
– Problems: Risk of nerve compression, pressure sores, and potential challenges in anesthesia and ventilation.
– Prevention: Careful padding to protect bony prominences, regular repositioning, and collaboration between anesthesia and surgical teams to address any ventilation issues.
In all positions, close communication and collaboration between the anesthesia and surgical teams are crucial for patient safety. Frequent monitoring, proper padding, vigilant attention to pressure points, and adherence to established protocols for each position are essential preventive measures. Preoperative assessment and patient-specific considerations also play a vital role in minimizing the risks associated with these positions.