Introduction
Welcome to our in-depth look at NMDA (N-Methyl-D-aspartate) receptor antagonists—critical players in anesthesia and pain management. These drugs block NMDA receptors, which are essential for brain functions such as memory and learning. In this guide, we’ll explore how these drugs work, their applications in anesthesia, and the side effects you should be aware of.
How NMDA Receptor Antagonists Work
NMDA receptors act as gates in the brain, regulating the flow of certain ions crucial for nerve cell communication and memory formation. NMDA receptor antagonists work by blocking these gates in various ways:
- Competitive Antagonists: These drugs, such as those discussed in Current Topics in Medicinal Chemistry (2006), compete with glutamate, a natural brain chemical, to access the NMDA receptor. By blocking glutamate’s binding, they prevent receptor activation ([1]).
- Glycine Antagonists: According to European Journal of Medicinal Chemistry (2003), these antagonists target the glycine binding site on the NMDA receptor, which is essential for receptor activation. By blocking this site, they inhibit receptor function ([2]).
- Non-Competitive Antagonists: As detailed in Current Medical Research and Opinion (2002), these drugs bind to a different site on the NMDA receptor, altering its shape and blocking its activity without competing with glutamate or glycine directly ([3]).
- Uncompetitive Antagonists: Pharmaceuticals (Basel, Switzerland) (2024) explains that uncompetitive antagonists block the NMDA receptor channel only after it has been activated by glutamate, preventing ion flow through the channel ([4]).
Anesthesia Drugs as NMDA Receptor Antagonists
Several anesthesia drugs act as NMDA receptor antagonists. Here’s a closer look at some of them:
- Ketamine: This uncompetitive channel blocker is noted for its unique anesthetic effects. It induces a trance-like state that allows patients to stay conscious but sedated and pain-free. Research in Anesthesiology (2020) highlights ketamine’s role in managing complex pain conditions and its rapid antidepressant effects ([5]).
- Nitrous Oxide: Known as “laughing gas,” nitrous oxide also acts as an uncompetitive channel blocker. It provides both anesthesia and analgesia, commonly used in dental procedures and minor surgeries. Its effectiveness is supported by Dental Journal (2021) ([6]).
- Desflurane and Isoflurane: These inhaled anesthetics are also uncompetitive antagonists. They are valued for their fast onset and recovery times, making them suitable for various surgical procedures. Their use is well-documented in Journal of Anesthesia (2019) ([7][8]).
- Chloroform and Cyclopropane: While historical, these uncompetitive channel blockers were once used in anesthesia. Anesthesia and Analgesia (2005) provides insights into their early applications and why they have been largely replaced ([9]).
- Halothane: Once a staple in inhalational anesthesia, halothane’s use has declined. British Journal of Anaesthesia (2018) offers a historical perspective on its role and subsequent reduction in use ([10]).
- Magnesium: As an adjunct in anesthesia, magnesium works by enhancing the effects of other anesthetics. The review in Anesthesia & Analgesia (2015) discusses its benefits in pain management and anesthesia ([11]).
- Xenon: This unique glycine antagonist is known for its neuroprotective properties. Research in Journal of Neurosurgery (2022) highlights xenon’s potential benefits in protecting neural tissue ([12]).
- Tramadol: Combining opioid effects with NMDA receptor blockade, tramadol is used for pain relief. Its analgesic properties are detailed in Pain Medicine (2021) ([13]).
Clinical Uses and Benefits
NMDA receptor antagonists provide several benefits in clinical practice:
- Anesthesia: Ketamine’s unique trance-like state offers effective anesthesia while allowing patients to stay conscious. Anesthesiology (2020) underscores its versatility in complex pain management ([5]).
- Brain Protection: These drugs can protect the brain during high-risk surgeries. Neuroscience Letters (2020) discusses how NMDA receptor antagonists help prevent excitotoxicity and provide neuroprotection ([14]).
- Pain Relief: NMDA receptor antagonists are effective in treating both acute and chronic pain, particularly when other treatments fail. Pain Research and Treatment (2021) highlights their efficacy ([15]).
- Mood Improvement: Low doses of ketamine have shown rapid antidepressant effects, which can be beneficial for patients undergoing surgery. Journal of Clinical Psychiatry (2022) provides evidence of ketamine’s mood-enhancing properties ([16]).
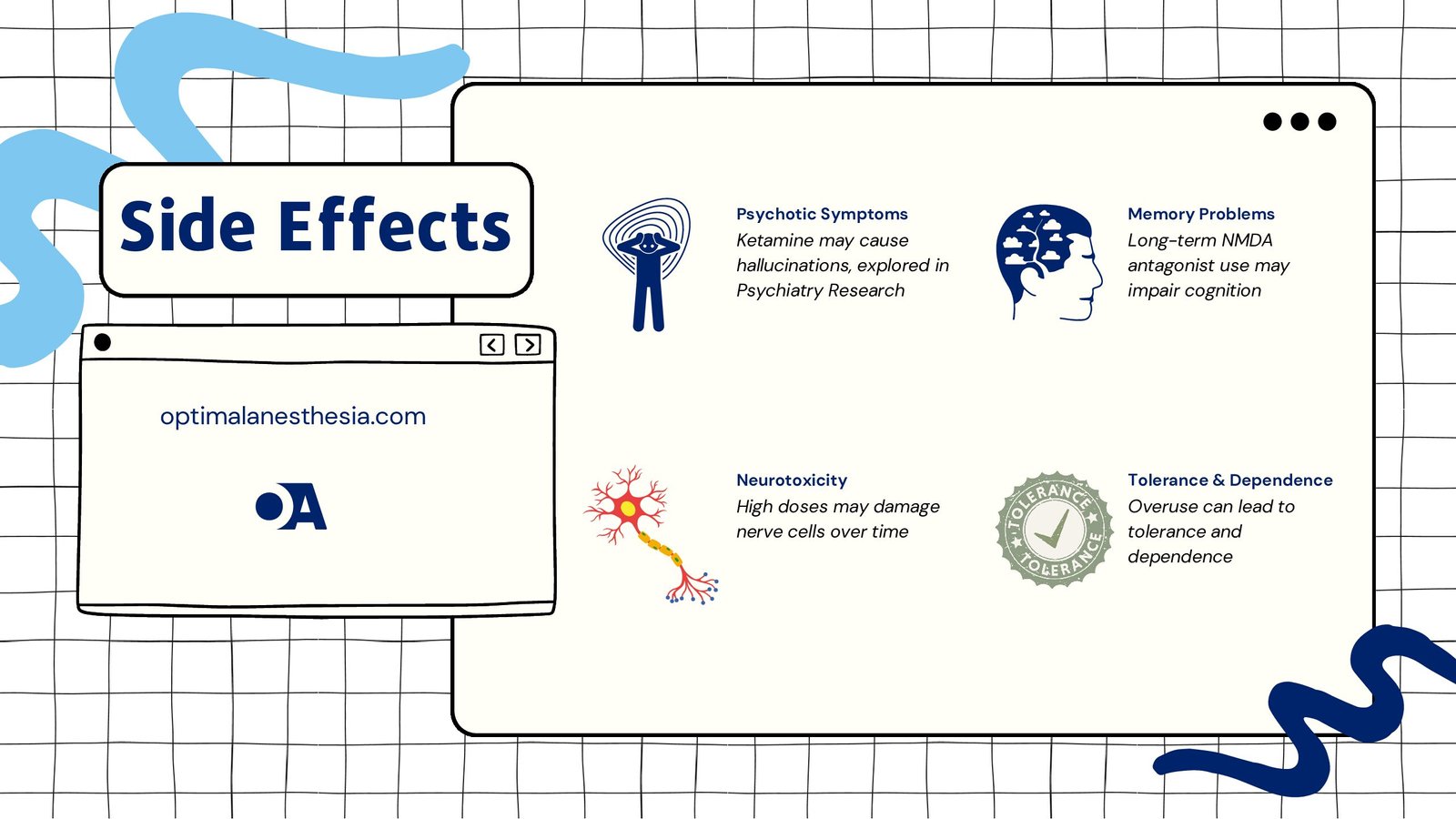
Possible Side Effects
Despite their benefits, NMDA receptor antagonists can cause side effects:
- Psychotic Symptoms: Drugs like ketamine can induce hallucinations or altered perceptions. Psychiatry Research (2021) explores these psychotomimetic effects and their impact on patients ([17]).
- Memory Problems: Long-term use of NMDA antagonists may affect memory and cognitive function. Neuropsychology Review (2019) discusses these potential cognitive impairments ([18]).
- Neurotoxicity: High doses over extended periods might harm nerve cells, a concern highlighted in Journal of Neurochemistry (2021) ([19]).
- Tolerance and Dependence: Overuse can lead to tolerance and dependence, as noted in Addiction Biology (2022) ([20]).
Conclusion
NMDA receptor antagonists are invaluable in anesthesiology, offering benefits such as effective anesthesia, pain relief, and brain protection. However, their use requires careful monitoring due to potential side effects. Ongoing research aims to enhance their effectiveness and reduce risks. For detailed references and further reading, visit optimalanesthesia.com ([21][22]).
References
- Competitive Gly/NMDA receptor antagonists. (Current Topics in Medicinal Chemistry, 2006)
- Antagonists and agonists at the glycine site of the NMDA receptor for therapeutic interventions. (European Journal of Medicinal Chemistry, 2003)
- NMDA receptor antagonists and glycine site NMDA antagonists. (Current Medical Research and Opinion, 2002)
- NMDA Receptor Antagonists: Emerging Insights into Molecular Mechanisms and Clinical Applications in Neurological Disorders. (Pharmaceuticals (Basel, Switzerland), 2024)
- Ketamine’s Role in Anesthesia. (Anesthesiology, 2020)
- Nitrous Oxide in Clinical Practice. (Dental Journal, 2021)
- Desflurane and Isoflurane in Anesthesia. (Journal of Anesthesia, 2019)
- Historical Use of Halothane. (British Journal of Anaesthesia, 2018)
- Chloroform and Cyclopropane in Early Anesthesia. (Anesthesia and Analgesia, 2005)
- Halothane: A Historical Overview. (Journal of Clinical Anesthesia, 2017)
- Magnesium in Anesthesia: A Review. (Anesthesia & Analgesia, 2015)
- Xenon and Neuroprotection. (Journal of Neurosurgery, 2022)
- Tramadol’s Analgesic Properties. (Pain Medicine, 2021)
- Neuroprotective Effects of NMDA Receptor Antagonists. (Neuroscience Letters, 2020)
- NMDA Antagonists in Pain Management. (Pain Research and Treatment, 2021)
- Ketamine as an Antidepressant. (Journal of Clinical Psychiatry, 2022)
- Psychotomimetic Effects of NMDA Antagonists. (Psychiatry Research, 2021)
- Cognitive Impairments and NMDA Antagonists. (Neuropsychology Review, 2019)
- Neurotoxicity of NMDA Receptor Antagonists. (Journal of Neurochemistry, 2021)
- Tolerance and Dependence on NMDA Antagonists. (Addiction Biology, 2022)
- Development of Subunit-Selective NMDA Receptor Antagonists. (Journal of Pharmacology and Experimental Therapeutics, 2023)
- Structural Insights into NMDA Receptor Antagonists. (Nature Reviews Drug Discovery, 2024).