Heat and Moisture Exchange Filters (HMEFs) are critical in maintaining the physiological conditions of inspired gases during anesthesia and mechanical ventilation. They replicate the heat and humidity provided by the upper respiratory tract, while also filtering out pathogens. This article reviews their components, working principles, advantages, and limitations, with references to support the discussion.
Components of an HME Filter
An HMEF comprises the following key parts, each designed to ensure efficient humidification and infection control:
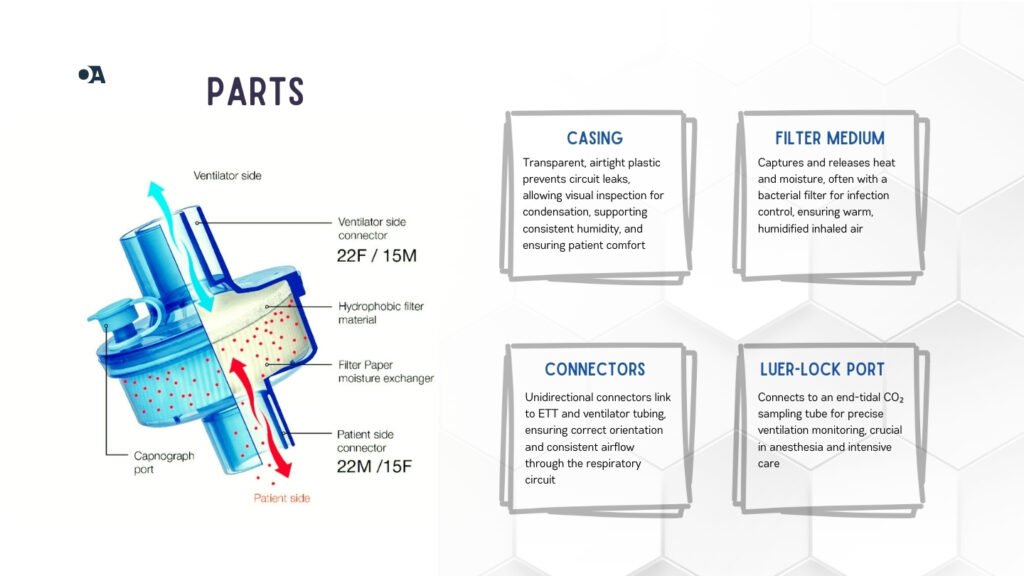
1. Casing
The casing is made of transparent, durable plastic that facilitates the visual inspection of internal components. The airtight design prevents gas leaks in the breathing circuit, ensuring patient safety.
2. Hygroscopic Filter Medium
The filter medium, typically constructed from treated materials such as cellulose, conserves heat and moisture from the patient’s exhaled air and releases them to the inspired air.
- Advanced HMEFs integrate high-efficiency bacterial and viral filters, which enhance protection against airborne pathogens.
3. Connectors
Unidirectional connectors allow seamless attachment to an endotracheal tube (ETT) or ventilator circuit, ensuring proper gas flow and secure connections.
4. Luer-Lock Port
This port enables connection to devices for capnography, facilitating accurate monitoring of ventilation and end-tidal carbon dioxide (EtCO₂) levels.
Principles of Operation
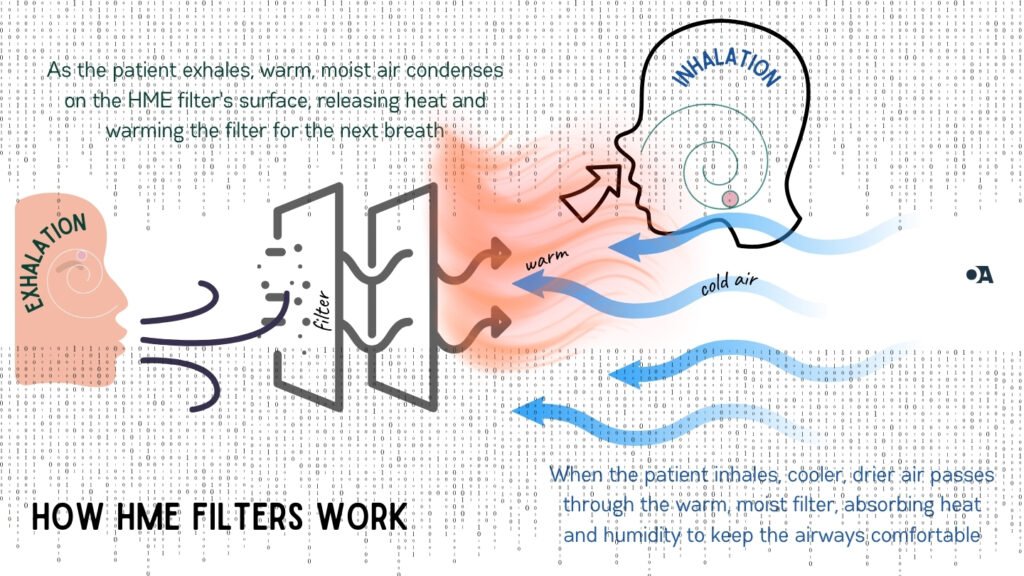
HMEFs capture heat and moisture from exhaled air during expiration and return it to inspired gases during the inhalation. This heat and moisture exchange process ensures that the inhaled air closely resembles physiological conditions, reducing the risk of airway complications.
- Expiration Phase: The hygroscopic filter medium absorbs moisture and heat from exhaled gases.
- Inspiration Phase: Dry, cool air from the ventilator picks up the retained heat and moisture, ensuring adequate humidification and warmth of the inspired gases.
Functions of HMEFs
Humidification
- Replaces the lost humidification when the upper airway is bypassed, preventing mucosal drying and airway irritation.
Temperature Regulation
- Conserves and provides heat to inspired gases, preventing hypothermia.
Filtration
- Traps bacteria and viruses, reducing the risk of nosocomial infections.
Airway Protection
- Mimics the upper airway’s function, ensuring respiratory mechanics’ integrity during mechanical ventilation.
Advantages of HMEFs
Cost-Effectiveness
- Disposable and affordable, reducing the risk of cross-contamination.
Ease of Use
- Operates passively without requiring external power or complex setup.
Compact Design
- Lightweight and compatible with various anesthesia circuits.
Effective Filtration
- High-efficiency particulate air (HEPA) filters can block particles as small as 0.2 microns.
Maintenance of Airway Conditions
- Provides adequate humidification and warmth for short-term ventilation.
Limitations of HMEFs
Added Dead Space
- Increases dead space in the breathing circuit, potentially affecting alveolar ventilation. This is particularly significant in neonates and pediatric patients.
Increased Airway Resistance
- May add up to 2–4 cmH₂O of resistance, challenging in patients with compromised respiratory mechanics.
Saturation Issues
- Accumulation of moisture or secretions can saturate the filter, leading to increased resistance and possible occlusion.
Limited Efficiency
- Prolonged use may lead to insufficient humidification compared to active humidifiers.
Best Practices for HMEF Use
Proper Selection
- Use HMEFs for short-term ventilation or anesthesia. Consider heated humidifiers for patients with high secretion loads or requiring long-term ventilation.
Monitoring
- Inspect filters regularly for moisture saturation, secretion buildup, or blockages.
Positioning
- Place the HMEF as close to the patient as possible for maximum efficiency.
Replacement Protocol
- Replace HMEFs every 24 hours or sooner in cases of contamination or increased resistance.
References
- Fischer, C., Bohn, D., & Kavanagh, B. P. (2011). The use of heat and moisture exchangers in ventilated patients to prevent hypothermia. Critical Care Medicine, 39(3), 510–518.
- Kelly, F. E., & Fong, J. J. (2015). Heat and moisture exchangers in ventilatory support: Benefits and limitations. Critical Care, 19(1), 314.
- Taylor, L. A., & Hewitt, M. A. (1998). Breathing system filters and heat moisture exchangers in anesthesia. British Journal of Anaesthesia, 91(2), 249–254.
- Pingleton, S. K., & Joyce, J. (2001). The role of HMEs in reducing complications in mechanical ventilation. Respiratory Care, 43(10), 1159–1165.
- HSI Medical. Heat Moisture Exchanger Filter (HMEF). Available at: https://www.hsi-med.com. Accessed November 2024.
- A-M Systems. Hydromax Heat & Moisture Exchange (HME) Filter. Available at: https://www.a-msystems.com. Accessed November 2024.
- Tri-anim Health Services. Heat Moisture Exchanger Filter HMEF, Humid-Vent Compact. Available at: https://www.tri-anim.com. Accessed November 2024.
- Intersurgical. HMEs and HMEFs for use in hospitals and at home. Available at: https://www.intersurgical.com. Accessed November 2024.