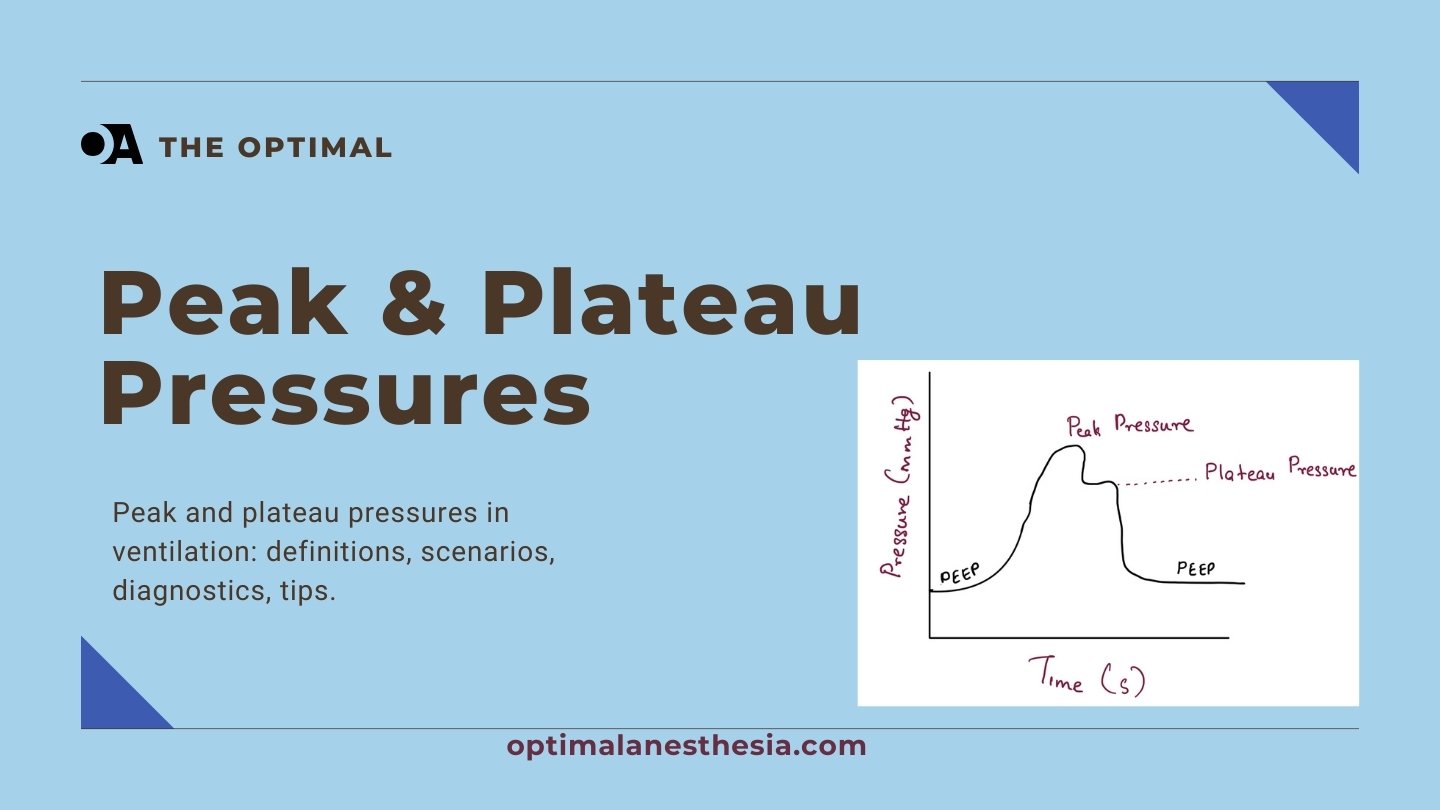
Peak Airway Pressure (Ppeak)
Ppeak represents the maximum pressure exerted by the ventilator to overcome both airway and alveolar resistance during inspiration. It is measured directly on the ventilator display during the inspiratory phase. Typically, the normal value for Ppeak is less than 35 cm H2O in mechanically ventilated patients (Respiratory Care, 2014). Elevated Ppeak can indicate increased airway resistance or mechanical obstruction, which may necessitate adjustments to ventilator settings or interventions to resolve the underlying issue.
Plateau Pressure (Pplat)
Pplat reflects the pressure remaining in the lung after tidal volume delivery, measured during an inspiratory hold maneuver when airflow is zero. The normal value for Pplat should ideally be less than 30 cm H2O to minimize the risk of ventilator-induced lung injury (VILI) (Critical Care Medicine, 2020). High Pplat suggests poor lung compliance, which can be seen in conditions like Acute Respiratory Distress Syndrome (ARDS) or pulmonary fibrosis (Critical Care (London, England), 2023).
Clinical Importance
Assessing Respiratory Mechanics
Ppeak is a crucial indicator of airway resistance and potential mechanical obstructions. An elevated Ppeak with a normal Pplat suggests increased airway resistance due to factors such as kinks in the ventilator circuit, fluid accumulation, or mucous plugging (Respiratory Care, 2005). Conversely, Pplat provides insight into lung and thoracic cavity compliance. High Pplat can indicate poor lung compliance, which may be due to conditions like pneumonia or pulmonary edema (American Journal of Respiratory and Critical Care Medicine, 2020).
Optimizing Ventilator Settings
Maintaining Pplat below 30 cm H2O is essential to prevent alveolar overdistension and VILI (Critical Care Medicine, 2023). Adjustments to tidal volume, positive end-expiratory pressure (PEEP), and inspiratory-to-expiratory ratio can help manage elevated Pplat. Ppeak should also be monitored and adjusted to address issues with airway resistance (Critical Care (London, England), 2024).
Identifying and Managing Complications
Elevated Ppeak with normal Pplat indicates issues with airway resistance, while high Pplat suggests problems with lung compliance. Common causes and solutions for these abnormalities include:
- High Peak Pressure / Normal Plateau Pressure:
- Kink in the Circuit: Examine and straighten the ventilator tubing (Frontiers in Physiology, 2022).
- Fluid Accumulation: Clear fluid from the circuit (Frontiers in Physiology, 2022).
- Biting the Endotracheal Tube (ETT): Increase sedation or insert a bite block (Frontiers in Physiology, 2022).
- Small ETT with Biofilm Formation: Consider changing out the tube (Frontiers in Physiology, 2022).
- High Flow Rate or Tidal Volume: Adjust ventilator settings (Frontiers in Physiology, 2022).
- Ventilatory Asynchrony: Increase sedation (Frontiers in Physiology, 2022).
- Laryngospasm or Bronchospasm: Administer steroids or epinephrine (Frontiers in Physiology, 2022).
- Mucous Plugging: Clear out the ETT (Frontiers in Physiology, 2022).
- Foreign Body: Remove the obstruction (Frontiers in Physiology, 2022).
- High Peak Pressure and High Plateau Pressure:
- Pneumonia: Obtain a chest X-ray, respiratory cultures, and start antibiotics (Anaesthesiology Intensive Therapy, 2015).
- Pulmonary Edema: Diurese and adjust PEEP settings (Anaesthesiology Intensive Therapy, 2015).
- Auto PEEP: Adjust PEEP, tidal volumes, or inspiratory-to-expiratory ratio. Consider sedation and manual ventilation if severe (Anaesthesiology Intensive Therapy, 2015).
- Right Main Stem Intubation: Retract the ETT slightly (Anaesthesiology Intensive Therapy, 2015).
- Pneumothorax: Evaluate with ultrasound or chest X-ray, then decompress and place a chest tube (Anaesthesiology Intensive Therapy, 2015).
- Atelectasis or Pulmonary Fibrosis: Adjust ventilation strategies accordingly (American Journal of Respiratory and Critical Care Medicine, 2020).
Advanced Considerations
Esophageal Pressure Monitoring
Esophageal pressure monitoring can provide a more accurate assessment of transpulmonary pressure, which may be particularly useful in patients with acute respiratory failure (Critical Care Medicine, 2006). This method estimates pleural pressure and helps gauge lung distending pressure more precisely.
Ventilation Modes and Pressure Measurements
Different ventilation modes affect peak and plateau pressures. Pressure-controlled ventilation (PCV) may result in lower peak airway pressures compared to volume-controlled ventilation (VCV) in certain settings (Journal of Minimally Invasive Gynecology, 2010). Airway pressure release ventilation (APRV) may offer benefits in maintaining lung elastance and oxygenation, particularly in extrapulmonary lung injury cases (Intensive Care Medicine Experimental, 2015).
Dynamic vs. Static Measurements
Static measurements like Pplat may underestimate the maximum pressure experienced by vulnerable lung units during dynamic inflation. Dynamic factors such as flow amplitude, inspiratory time fraction, and cycling frequency are important in evaluating the risk of VILI (American Journal of Respiratory and Critical Care Medicine, 2020).
Conclusion
Understanding and monitoring Peak Airway Pressure and Plateau Pressure are vital for optimizing mechanical ventilation, diagnosing respiratory complications, and preventing VILI. Clinicians must consider various factors, including patient characteristics, ventilation mode, and measurement methods, to tailor interventions effectively. Advanced techniques like transpulmonary pressure monitoring and dynamic assessments can provide more accurate evaluations and guide better ventilatory strategies.
References
- Respiratory Care, 2014. “Respiratory mechanics in mechanically ventilated patients.”
- Critical Care Medicine, 2020. “Mean Airway Pressure As a Predictor of 90-Day Mortality in Mechanically Ventilated Patients.”
- Critical Care (London, England), 2023. “Advanced respiratory mechanics assessment in mechanically ventilated obese and non-obese patients with or without acute respiratory distress syndrome.”
- Anaesthesiology Intensive Therapy, 2015. “Transpulmonary pressure monitoring during mechanical ventilation: a bench-to-bedside review.”
- Frontiers in Physiology, 2022. “Static and Dynamic Measurements of Compliance and Driving Pressure: A Pilot Study.”
- Journal of Minimally Invasive Gynecology, 2010. “Pressure-controlled vs volume-controlled ventilation during laparoscopic gynecologic surgery.”
- Intensive Care Medicine Experimental, 2015. “The effects of airway pressure release ventilation on respiratory mechanics in extrapulmonary lung injury.”
- American Journal of Respiratory and Critical Care Medicine, 2020. “Static and Dynamic Contributors to Ventilator-induced Lung Injury in Clinical Practice. Pressure, Energy, and Power.”
- Critical Care Medicine, 2006. “Esophageal and transpulmonary pressures in acute respiratory failure.”
- Critical Care (London, England), 2024. “Driving pressure of respiratory system and lung stress in mechanically ventilated patients with active breathing.”
- Respiratory Care, 2005. “Ventilator graphics and respiratory mechanics in the patient with obstructive lung disease.”