Introduction
Ketamine is a versatile medication with a fascinating history, complex pharmacology, and a wide range of clinical applications. In this article, we will delve into the various aspects of ketamine, including its history, structure-activity relationship, mechanism of action, pharmacokinetics, clinical uses, and potential side effects.
History of Ketamine
| Year of Discovery | Inventors | Initial Use | FDA Approval | Controlled Substance |
|---|---|---|---|---|
| 1962 | Calvin Stevens and Parke-Davis Laboratories | Anesthetic agent for humans and animals | Approved in 1970 | Schedule III |
Structure-Activity Relationship of Ketamine
Ketamine is a water-soluble molecule with an asymmetric carbon atom, resulting in two optical isomers: S(1)-ketamine and R(2)-ketamine. The racemic form of ketamine is most commonly used, although S(1)-ketamine is clinically available. Here’s a summary of the key differences between these isomers:
| Property | S(1)-Ketamine | R(2)-Ketamine | Racemic Ketamine |
|---|---|---|---|
| Analgesic Potency | More intense | Less intense | Intermediate |
| Metabolism and Recovery | More rapid | Slower | Intermediate |
| Salivation | Less | More | Intermediate |
| Emergence Reactions | Lower incidence | Higher incidence | Intermediate |
| Fatigue and Cognitive Impairment | Less | More | Intermediate |
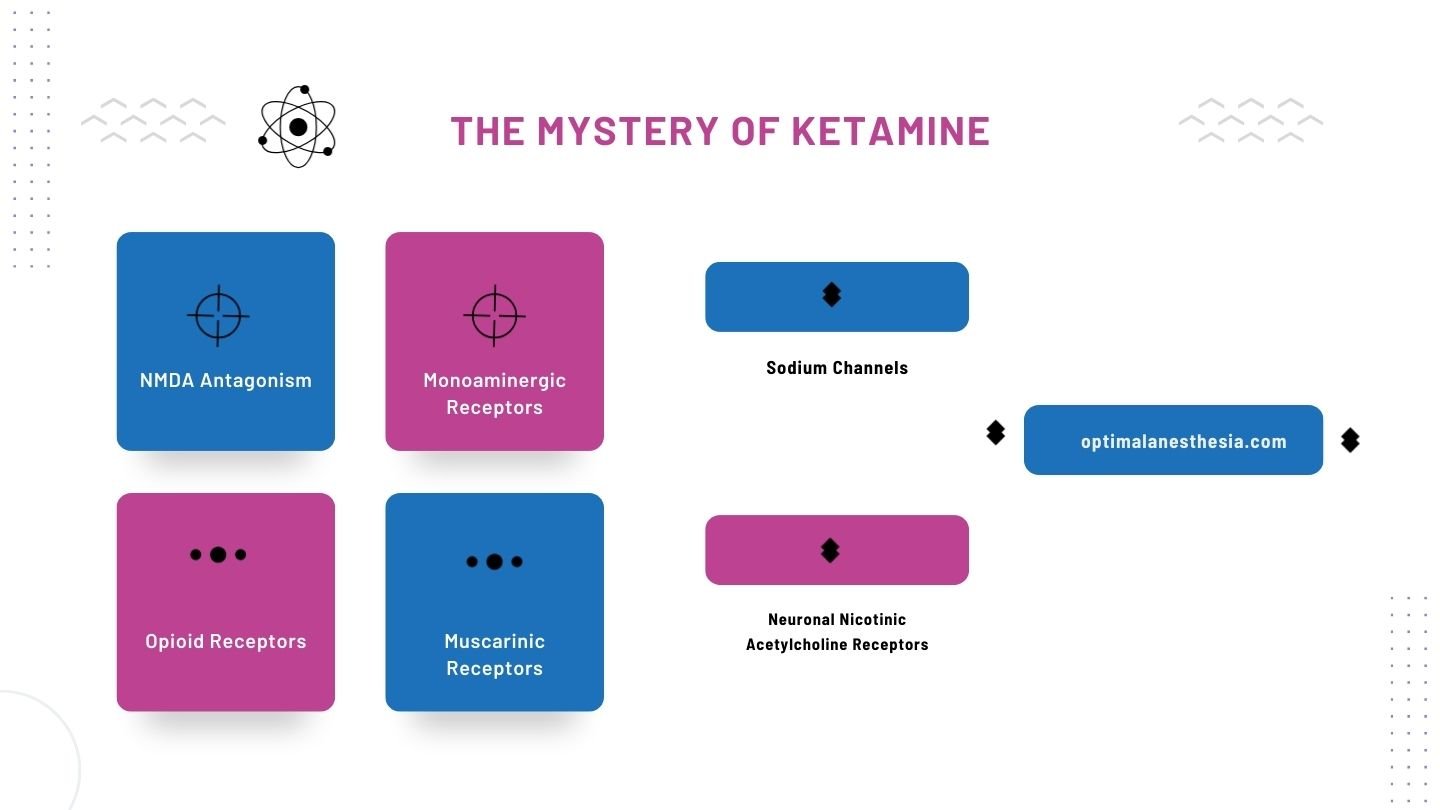
Mechanism of Action
Ketamine interacts with various central nervous system receptors, although its precise mechanism of action is not fully understood. Here are the key receptors and actions associated with ketamine:
N-Methyl-d-Aspartate (NMDA) Receptor Antagonism:
- Ketamine binds non-competitively to the phencyclidine recognition site on NMDA receptors.
- Inhibits activation of NMDA receptors by glutamate.
- Decreases presynaptic release of glutamate.
- S(1)-ketamine exhibits the greatest affinity for NMDA receptors.
Opioid Receptors:
- Ketamine interacts with mu (m), delta (d), and kappa (k) opioid receptors.
- May act as an antagonist at mu receptors and an agonist at kappa receptors.
Monoaminergic Receptors:
- Ketamine may activate descending inhibitory monoaminergic pain pathways.
Muscarinic Receptors:
- Ketamine partially antagonizes muscarinic receptors.
- Produces anticholinergic symptoms, such as emergence delirium and sympathomimetic actions.
Sodium Channels:
- Interacts with voltage-gated sodium channels, sharing a binding site with local anesthetics.
Neuronal Nicotinic Acetylcholine Receptors:
- Interacts with a7-type nicotinic acetylcholine receptors, which may contribute to its analgesic effects.
Pharmacokinetics of Ketamine
Ketamine exhibits unique pharmacokinetic properties:
| Property | Description |
|---|---|
| Onset of Action | Rapid |
| Duration of Action | Short |
| Lipid Solubility | High |
| Peak Plasma Concentrations | Within 1 minute after IV administration |
| Volume of Distribution (Vd) | 3 L/kg |
| Elimination Half-Time | 2 to 3 hours |
| Metabolism | Liver metabolism to active metabolite norketamine and inactive glucuronide metabolites |
| Renal Excretion | Less than 4% excreted unchanged in urine |
Clinical Uses of Ketamine
Ketamine finds diverse applications in the medical field:
Analgesia: Ketamine provides intense analgesia, particularly for somatic pain, and can be used as an adjunct to opioid analgesia.
Induction of Anesthesia: It is widely used for rapid induction of anesthesia, maintaining airway reflexes.
Special Considerations:
- Ketamine can be used in acutely hypovolemic patients, but caution is needed in patients with coronary artery disease.
- It is a preferred choice for rapid IV induction in patients with asthma due to its bronchodilatory effects.
Additional Uses: Ketamine has shown potential in opioid tolerance reversal, psychiatric disorders, and restless leg syndrome.
Side Effects of Ketamine
Ketamine administration can lead to various side effects and physiological responses, affecting multiple organ systems, including the central nervous system, cardiovascular system, and airway. These side effects include alterations in cerebral blood flow, cardiovascular stimulation, and bronchodilatory effects, among others.
Conclusion:
Ketamine’s rich history, complex pharmacology, and broad clinical utility make it a remarkable drug in the world of medicine. Its unique properties continue to make it a subject of interest and research across various medical disciplines. Understanding its mechanisms, applications, and potential side effects is crucial for its safe and effective use in clinical practice.