- Thyroid disease is common, especially in women and older individuals.
- Patients undergoing surgery may have concomitant thyroid disease.
- Most well-compensated thyroid disease patients don’t need special preoperative considerations.
- Patients with newly diagnosed thyroid disorders around the time of surgery should discuss risks and benefits.
- Preoperative measurement of TSH (thyroid-stimulating hormone) is generally unnecessary in routine preoperative medical consultations.
- If a patient’s history and physical examination suggest thyroid disease, diagnosis may be pursued for perioperative management.
- For patients with known thyroid disease taking medication, routine monitoring of thyroid function is recommended at least annually.
- Additional testing before surgery is usually unnecessary if the patient is on a stable dose of medication and euthyroidism was documented within the past three to six months.
HYPOTHYROIDISM:
Clinical Manifestations of Hypothyroidism Impacting Perioperative Outcome:
- Hypothyroidism affects multiple bodily systems, influencing perioperative outcomes.
- It leads to decreased cardiac output due to reduced heart rate and contractility.
- Respiratory muscle weakness and decreased pulmonary responses result in hypoventilation.
- Hypothyroidism causes decreased gut motility, leading to constipation and ileus.
- Various metabolic abnormalities can occur, including hyponatremia, increased serum creatinine, and reduced drug clearance.
- Patients with hypothyroidism often experience normochromic, normocytic anemia.
Severity of Hypothyroidism Definitions:
- Severe Hypothyroidism: Includes patients with myxedema coma, severe clinical symptoms, or very low levels of total thyroxine (T4) or free T4.
- Moderate Hypothyroidism: Encompasses patients with elevated thyroid-stimulating hormone (TSH) and low free T4, without severe symptoms.
- Mild Hypothyroidism: Includes patients with subclinical hypothyroidism, characterized by elevated TSH and normal free T4.
Surgical Outcomes Based on Hypothyroidism Severity:
- Mild (subclinical) hypothyroidism generally shows few adverse surgical outcomes.
- Moderate hypothyroidism may lead to perioperative complications like ileus, hypotension, hyponatremia, and impaired wound healing.
- Severe hypothyroidism is associated with intraoperative hypotension, cardiovascular collapse, and heightened sensitivity to anesthesia.
Management of Hypothyroidism in Surgery:
- Subclinical hypothyroidism typically doesn’t require surgery postponement.
- For moderate hypothyroidism, elective surgery may be postponed until euthyroid state restoration, but urgent surgery can proceed with caution.
- Severe hypothyroidism necessitates treatment and may require postponement of elective surgery.
- In hospitalized or critically ill patients, assessing thyroid function can be challenging.
- Nonurgent surgeries should be postponed in critically ill patients with nonthyroidal illness.
- In urgent surgery cases with suspected hypothyroidism, thyroid hormone replacement is considered.
- Repletion of thyroid hormone should be cautious and guided by monitoring thyroid function.
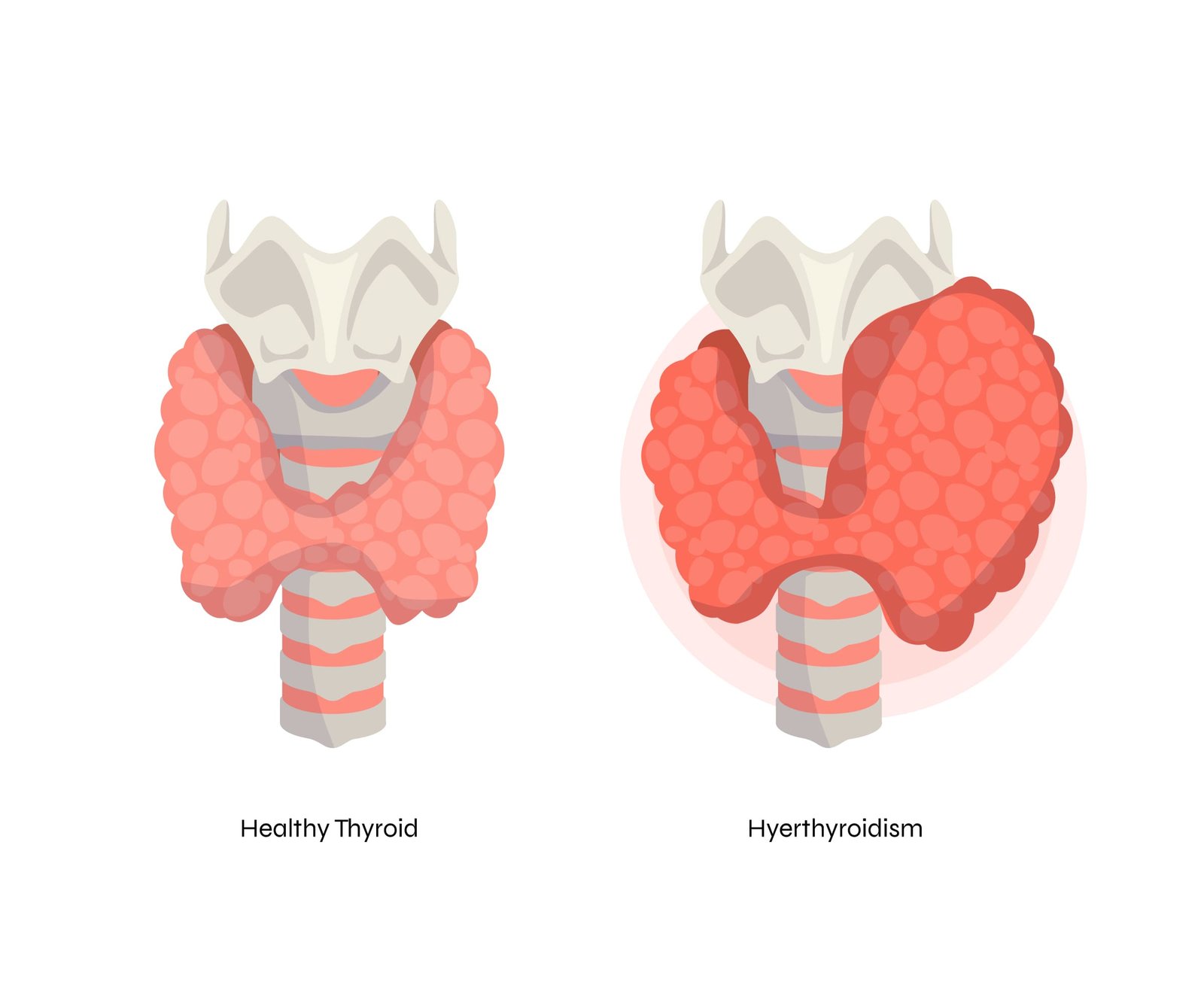
HYPERTHYROIDISM:
Clinical Manifestations:
- Hyperthyroidism affects various bodily systems.
- Increased cardiac output, heart rate, and widened pulse pressure.
- Atrial fibrillation is common, especially in older patients.
- Dyspnea may occur due to increased oxygen consumption.
- Weight loss results from increased calorigenesis and gut motility.
Management:
- Management decisions depend on the severity of hyperthyroidism.
- Subclinical hyperthyroidism can proceed with elective surgeries.
- Overt hyperthyroidism should be controlled before elective surgery.
- Urgent surgery in hyperthyroid patients requires preoperative treatment.
- Consider evaluation for cardiopulmonary disease and monitor for complications.
- Use beta blockers (e.g., atenolol) for rate control in some patients.
- Thionamides (e.g., methimazole) are used for postoperative control.
- Iodine (SSKI) may be added in severe hyperthyroidism.
- Extreme caution with iodine in toxic adenoma/multinodular goiter.
- Consider using iopanoic acid where available.
- Some patients intolerant to thionamides can use beta blockers and iodine.
- Thyroid storm is a risk during surgery and in the first 18 hours post-surgery.