- Epistaxis (Nasal Bleeding): Epistaxis is a common complication of nasotracheal intubation due to the manipulation of delicate nasal tissues. The reported incidence varies widely, with studies indicating rates between 15% to 35%. The severity of bleeding can range from mild oozing to more significant bleeding requiring intervention.
- Mucosal Injury: Mucosal injury is another frequent complication, characterized by damage to the nasal mucosa during tube insertion. The incidence of mucosal injury has been reported to be around 10% to 30%, with variations depending on the patient population and intubation technique used.
- Trauma to Nasal Structures: Trauma to nasal structures, including septal deviation or fracture, is less common but can occur during intubation. The reported incidence of such trauma is relatively lower, around 1% to 5%.
- Misplacement of Tube: Misplacement of the endotracheal tube into the esophagus or bronchus is a serious complication. The incidence varies depending on factors like operator experience and confirmation methods. Reported rates of misplacement range from 1% to 10%.
- Difficult Intubation: Difficult intubation refe
- rs to challenges encountered during tube insertion due to anatomical variations or other factors. The incidence of difficult intubation during nasotracheal intubation has been reported in the range of 10% to 20%.
- Nasopharyngeal Trauma: Trauma to the nasopharynx, including damage to the adenoids or posterior structures, can occur during intubation. The reported incidence of nasopharyngeal trauma ranges from 5% to 15%.
- Hemodynamic Changes: The manipulation of the nasal passage and subsequent sympathetic stimulation can lead to hemodynamic changes such as increased heart rate and blood pressure. These changes are generally transient. The reported incidence varies and can affect a significant portion of patients undergoing nasotracheal intubation.
- Patient Discomfort: Patient discomfort is a common concern, as nasotracheal intubation can be unpleasant. The incidence of patient discomfort varies widely and is influenced by individual pain tolerance and preoperative anxiety levels.
It’s important to note that these incidence rates are estimates and can vary based on factors like patient population, clinical setting, and procedural techniques. Additionally, advancements in equipment and intubation techniques may impact the incidence of complications. To minimize these complications, the routine use of transnasal flexible videoendoscopy (TVE) before nasotracheal intubation can provide critical insights into nasal anatomy, mucosal condition, and potential obstacles, allowing anesthesiologists to tailor their approach and mitigate these risks more effectively.

The Crucial Need for Transnasal Flexible Videoendoscopy Before Nasotracheal Intubation:
Navigating the realm of airway management requires a deep understanding of critical procedures, and among them, transnasal flexible videoendoscopy stands out as a pivotal step before nasotracheal intubation. Let’s break down the reasons why this procedure is an absolute necessity:
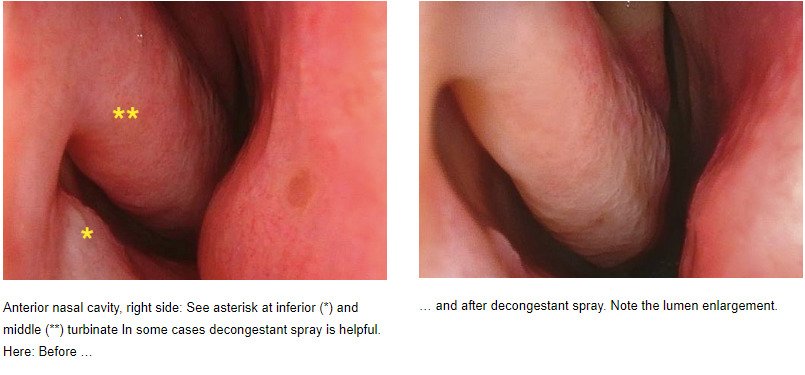
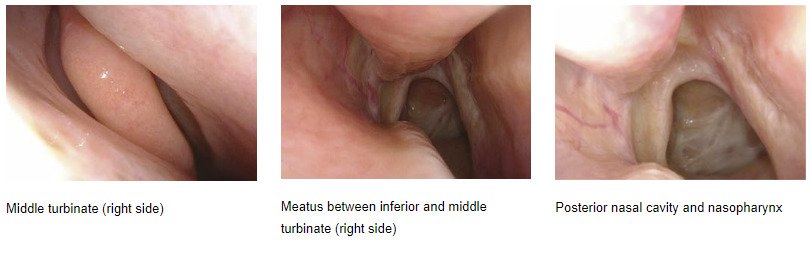
1. Enhanced Airway Evaluation: Transnasal flexible videoendoscopy provides a direct view of the larynx, allowing for a meticulous assessment of airway anatomy. This evaluation includes the size and shape of nasal passages, the position of the septum, and the presence of any obstructions that might complicate intubation.
2. Identification of Pathologies: By employing transnasal videoendoscopy, anesthesiologists can identify pre-existing pathologies that could hinder successful intubation. These could range from nasal polyps and tumors to anatomical variations, all of which impact the intubation process.
3. Optimal Nostril Selection: One of the critical decisions for nasotracheal intubation is selecting the appropriate nostril. Transnasal flexible videoendoscopy aids in this decision-making process by evaluating nasal patency, anatomical abnormalities, and the presence of pathologies, ensuring the optimal choice of nostril.
4. Mitigating Complications: Intubation via the nasal route can be accompanied by complications like bleeding, trauma, and difficulty in tube placement. Transnasal videoendoscopy minimizes these risks by offering a clear visualization of nasal passages and the larynx, allowing precise and careful tube navigation.
5. Proactive Patient Safety: Performing transnasal videoendoscopy before head and neck surgery proactively identifies potential challenges in the airway. This knowledge empowers anesthesiologists to prepare for difficult intubation scenarios, ensuring patient safety during surgery.
Incorporating Transnasal Flexible Videoendoscopy:
As you continue your journey as an anesthesiologist embracing the significance of transnasal flexible videoendoscopy is crucial.