As you delve into the realm of regional anesthesia techniques, it’s crucial to understand the nuances of advanced approaches, such as the adductor canal block (ACB). This technique has garnered increased interest due to its potential to preserve postoperative quadriceps strength while facilitating early mobilization after total knee replacement (TKR). Let’s embark on a journey through its evolution, relevant anatomy, benefits, concerns, and a fascinating variation known as the sub-sartorial plexus block.
Evolution of Adductor Canal Block:
Evolution of Adductor Canal Block:
- Foundation Laid (1993): The concept of ACB was initiated by van Der Wal and associates as an alternative to traditional saphenous nerve blocks for foot and ankle procedures.
- Anatomic Insights (2009): Horn and colleagues provided an anatomical basis for the ultrasound-guided approach to saphenous nerve blockade, marking a significant step forward.
- Knee Analgesia (2009): Manickam and colleagues introduced the idea of using saphenous nerve blockade in the adductor canal for knee joint analgesia.
- Addressing Fall Risk (2011): Sharma and team linked femoral nerve blocks used for knee analgesia with increased fall risk. This prompted the search for alternatives that spare motor strength.
- Advancements (2011): Lund and associates explored adductor canal block for post-knee surgery analgesia, introducing peri-neural catheters to the field. Simultaneously, Saranteas et al highlighted the saphenous nerve’s location within the adductor canal.
- Enhanced Alternative (2011): Karpoor and colleagues addressed muscle weakness concerns by implementing saphenous nerve block in the adductor canal, offering an effective alternative.
Relevant Anatomy:
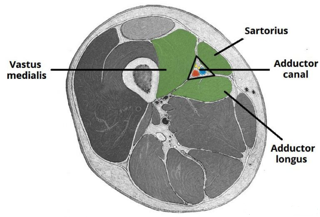
The adductor canal is a conical aponeurotic tunnel extending from the femoral triangle to the adductor hiatus. It transmits various neurovascular structures, including the femoral artery, vein, nerve to vastus medialis, and saphenous nerve. It is bordered by the sartorius, vastus medialis, and adductor muscles.
Benefits and Concerns:
Benefits:
- Targeted sensory blockade
- Limited quadriceps weakness for better ambulation and rehabilitation
- Facilitates assessment of compartment syndrome
Concerns:
- Possible vastus medialis weakness due to motor nerve blockade
- Local anesthetic induced myotoxicity (LAMT)
- Saphenous nerve entrapment with high volumes
- Spreading of local anesthetic to femoral triangle
- Potential injury to the saphenous nerve within the vastoadductor membrane

A) Cross-sectional anatomy of the saphenous nerve at the level of the thigh. The saphenous nerve (SaN) is positioned between the sartorius muscle (SM) and the vastus medialis muscle (VM), anterolateral to the femoral artery (FA) and vein (FV). AMM, adductor magnus muscles; GM, gracilis muscle; MRN, medial retinacular nerve.
(B) US anatomy of the sub-sartorial space at the mid-thigh.